Cervical Spine Surgery

The cervical spine
What is it?
The part of your spine that makes up the neck region is known as the cervical spine. This section is interesting because it’s composed of the first seven vertebrae in your spinal column, beginning just beneath your skull and concluding right above your upper back (thoracic spine).
The difference between the cervical spine and the other parts of the spine is its remarkable range of movement. This unique feature is thanks to two special vertebrae called the atlas and the axis, which are specifically crafted for rotation.
Although the cervical spine is very flexible, it is also at risk for injury from strong, sudden movements, such as whiplash-type injuries. This is due in part to the limited number of muscles located in the cervical area, combined with the fact the cervical spine has to support the weight of the head, which weighs an average of 10 – 13 pounds.
With its complex and intricate construct and the many stresses and forces that can be placed on it through trauma or even just daily activities, the cervical spine is at risk for developing a number of painful conditions.
Decompress and stabilize
Anterior Cervical Discectomy and Fusion
An anterior cervical discectomy and fusion (ACDF) is a combined surgical procedure that Dr. Washington performs to decompress spinal nerves and stabilize the cervical spine. The goal of ACDF is to relieve pain, numbness, and weakness in the neck, shoulder, and arms, and to provide stability in the cervical portion of the spine.
An ACDF is considered when there has been severe damage to the upper spine due to a fracture, a congenital anomaly, or a disc condition such as osteoarthritis or herniation. An ACDF is usually performed when a patient is experiencing debilitating pain because cervical nerves are being compressed or when there is excessive motion between the vertebrae of the cervical spine.
The Procedure
The surgery itself is made up of two parts:
1. Discectomy – The damaged disc is removed through the small incision that was made. This eliminates pressure on the compressed nerve, thus relieving the pain and other symptoms the compression causes.
2. Fusion – A bone graft or implant device is inserted in the empty space where the damaged disc was located to provide strength and stability to the area.
The procedure is performed using a minimally invasive technique in which a small incision is made in the front (anterior) of the neck, which gives him direct access to the damaged disc through a relatively uncomplicated pathway. The disc is removed through the incision and then a bone graft or an implant device is inserted into the empty space where the damaged disc was to provide strength and stability to the area. The procedure may also involve removing part of the vertebra or widening the spinal canal to give the spinal cord more space if neurological symptoms from spinal cord compression are present.
While it takes several months for the bones to fully fuse, most patients feel better within a few weeks of the surgery.

Motion preserving
Cervical Disc Replacement
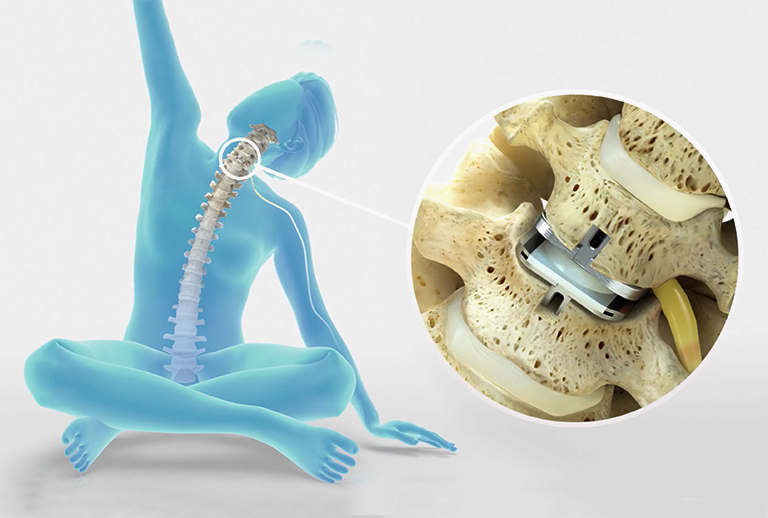
The best kind of surgery is no surgery at all, but for neck and arm pain that has failed nonoperative treatment, motion-sparing surgery such as cervical disc replacement may be an excellent option. This procedure allows for continued motion in the spine, compared to fusion which restricts motion and can put strain on the rest of the neck.
Cervical disc replacement is a type of joint replacement procedure in which an artificial disc is placed in the space between the vertebrae after the damaged disc has been removed. Cervical disc replacement is usually recommended for patients who have disc herniation, neck injury, or degenerative disc disease causing chronic pain that hasn’t been relieved through non-surgical treatments.
The Procedure
Cervical disc replacement is performed as an alternative to fusion surgery because it provides patients with numerous benefits, including preserved motion. The procedure is designed to relieve the pressure on your spinal cord or nerves causing the pain, numbness, and weakness that can radiate to your shoulder, arm, and hand.
During the procedure, the damaged disc is removed and replaced with an artificial one, which is designed to replicate the natural motion of the spine. After the damaged disc is removed, any bone spurs will be smoothed away and an artificial disc will be anchored in the empty space that is left.
Surgery from the back
Posterior Cervical Laminectomy & Fusion
Posterior cervical laminectomy and fusion is the general term used to describe the procedure of mending two or more cervical vertebrae through an incision in the back (posterior) of the neck.
The procedure removes portions of the cervical vertebrae (the lamina) that are causing compression of the spinal cord and nerves, followed by fusion of the adjacent vertebrae to restore spinal stability. A fusion usually involves placing a bone graft to provide stability and eliminate motion. The procedure is a common one for patients who have cervical spine fractures or instability.
The Procedure
During a posterior cervical laminectomy and fusion, an incision is made in the back of the neck and a section of the lamina, or the entire lamina is removed to eliminate the pressure on the spinal cord and nerve roots. The fusion is then performed by placing a bone graft or bone graft substitute along the sides of the injured section of the cervical spine. Over time, this bone graft fuses to provide healing and greater stability. Metal screws and rods are sometimes used in conjunction with the procedure to extend fusion and/or provide immediate stability, as well as increase the likelihood of successful fusion.


Relieving pressure
Cervical Laminoplasty
A cervical laminoplasty is a surgical technique that removes pressure from the spinal cord in the neck that can be due to various reasons, including degenerative changes, arthritis, bone spurs, disc herniation, fractures, or spinal stenosis.
The goal of laminoplasty is to relieve pressure caused by the narrowing of the spinal canal. This procedure immediately relieves pressure by creating more space for the spinal cord and nerve roots. The cervical canal narrowing can result in numbness, pain, and weakness of limbs, as well as difficulty in walking and if left untreated, even paralysis.
Performed through the back of the neck, a cervical laminoplasty is designed to retain the natural movement of the neck after surgery.
The Procedure
During a laminoplasty surgery, an incision is made in the back of the neck through which a small portion of the bony part of the spinal canal (called the lamina) is removed to enlarge the spinal canal, thereby relieving symptoms of nerve root compression. By enlarging the spinal canal, it can relieve symptoms of radiating pain or weakness, or numbness in the arm or hand. In a laminoplasty, more of the normal bone and ligaments remain intact, which provides a protective layer that lessens scar tissue formation on the dural sac after surgery.
Most patients are encouraged to begin walking in the hospital within a few hours of surgery once they have recovered from the anesthesia. It is normal for continued pain immediately after surgery, particularly around the incision, and as the inflammation around the offending nerve root slowly decreases. Outpatient physical therapy may be prescribed to help with pain and inflammation and to regain function and control of the neck muscles. Recovery times vary for every patient, but on average, patients recover within two to four weeks.